Considering a switch to an EHR system? You are not alone; a lot of healthcare providers are now abandoning paper charts and lengthy workflows for digital ease. But before you jump, there’s one thing you need to get right that is EHR implementation cost.
The costs of implementing an EHR are multifaceted. Consider setup fees, hardware, training, workflow interruptions, and even internet upgrades. And with the EHR market expected to grow to an estimated $45.9 billion by 2033 (Market vs Media), digital health records are in the lead for the long haul.
This guide gives you the full picture if you’re a clinic, hospital, or private practice trying to go digital. No fluff, just facts. So let’s unpack it all so you can make the right investment. Let’s get started.
What Is An EHR?
Electronic Health Record (EHR) is a digital version of a patient’s paper chart. To be precise, EHR is a real-time, patient-centered record that is instantly and securely shared with authorized users. It consists of everything from medical history, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and lab results.
EHRs do far more than just store information. They are designed to facilitate the delivery of health care. They can analyze data over time to target patients for preventive visits, leading to better treatment outcomes. And because it’s digital, it means less paperwork, less time, and a reduction of unnecessary mistakes.
When managing a small clinic or a hospital, each organization needs to work with an all-in-one EHR system, the center point that runs business functions, serves patients better, and stays compliant with health regulations.
Understanding The Cost Of EHR Implementation
When it comes to EHR implementation, cost is not as simple as a price tag. The Software Path 2022 EHR Report estimates that the average cost of EHR software is $1,200 annually per user, but this is only the starting point. For example, a small clinic with three users can anticipate paying roughly $300 per month. But that number barely scratches the surface.
Choosing the right deployment model is one of the biggest financial obstacles you will have to overcome when implementing an EHR system. The upfront and ongoing costs can differ widely depending on whether you choose a cloud-based or on-premise solution.
Let’s take a closer look at what each option costs:
1. On-Premise EHR
An on-premise EHR is a system in which your healthcare organization buys a perpetual license and hosts the entire system on internal servers. This method provides you with more leverage over your data and IT infrastructure, but it is extremely costly.
Here’s what you need to budget for on-premise EHRs:
- One-time licensing fee (typically large upfront)
- Server and storage hardware
- IT staff for installation and maintenance
- Data backup and recovery systems
- Security infrastructure
In the first year, costs can go as high as $85,000, according to industry estimates, mainly because you also have to consider covering ongoing hardware maintenance, setting up the software, and necessary upgrades.
This model is ideal for large practices or healthcare facilities with a strong internal IT team available to maintain the system.
2. Cloud-Based EHR
Cloud-based EHR systems keep all the data on the vendor’s servers and provide access through the internet. This approach has lower upfront costs and is a cost-effective option for small clinics or organizations with lower IT infrastructure.
Key costs associated with cloud EHR systems:
- Monthly or annual subscription fees
- User-based pricing (costs increase with more users)
- Optional one-time setup or implementation fees
- Third-party integrations (if needed)
Since the vendor takes care of hosting, storage, security, and routine updates, you won’t need to buy or manage physical servers or complex infrastructure. Your costs could increase as your practice expands, especially if your vendor charges per user.
For instance, certain EHR vendors, such as eClinicalWorks, charge extra fees when your practice has more than nine providers.
Quick Comparison: Cloud vs. On-Premise Direct Costs
| Deployment Method | Cloud-Based (Vendor-Hosted) | On-Premise (Self-Hosted) |
|---|---|---|
| Initial Cost | Lower, subscription-based | Higher, one-time license fee |
| Scalability | Easy, the cost grows with users | Complex, may need new servers |
| Hardware Costs | Minimal | High (servers, storage, etc.) |
| Maintenance | Vendor-managed | Self-managed IT and upkeep |
| Best For | Small to mid-size practices | Large practices with IT teams |
2. Indirect Costs
Indirect costs are the expenses that don’t appear upfront but still impact your budget, resources, and operations during and after EHR implementation. Unlike direct costs, such as purchasing software licenses or setting up hardware, indirect costs are less obvious but equally important to consider.
Direct costs such as software licensing and hardware setup are easy to spot, but indirect costs of EHR implementation often fly under the radar. Moreover, they can have significant repercussions on both your budget and day-to-day operations.
These hidden costs that aren’t specifically part of the EHR system pricing are integral to a smooth and sustainable transition. Let’s understand them in detail:
A) Downtime & Productivity Loss
Downtime is one of the most significant hidden costs of EHR implementation. Downtime refers to the temporary dip in performance and productivity that occurs as staff adjust to the new EHR system during its initial implementation phase.
These workflow interruptions are practically unavoidable, particularly in the first few days of implementation, as your staff acclimates to the new software system.
- Expect slower appointment handling.
- Patient volume may temporarily drop.
- Revenue may dip as your team spends more time learning the software.
Being proactive about this loss of productivity ensures that you will be financially prepared and minimizes frustration for staff and patients.
B) EHR System Maintenance & Technical Support
The job isn’t complete even after your EHR system has launched. You will still require ongoing support, maintenance, and updates to ensure everything is functioning properly.
These post-implementation costs often include:
- Regular software updates
- Vendor support or helpdesk access
- System monitoring and bug fixes
- Security patches and data backups
If your EHR is cloud-based, these services may already be part of your subscription, but it’s a good idea to confirm that you’re covered by your plan. For on-premise installations, this responsibility falls on your internal IT team, which puts pressure on your staffing and support costs.
Why do Indirect Costs Matter?
Overlooking these indirect costs can contribute to budget overspending and operational pain points. Integrating them into your EHR implementation plan will guarantee a smoother rollout and better system performance in the long run.
Pro Tip: Request a comprehensive breakdown of both direct and indirect costs from your EHR vendor prior to contract signature. That’s the best means to dodge surprises down the road.
3. Staff Related Costs
A significant but often underappreciated contributor to EHR implementation costs comes in the form of the staff training and support necessary for its adoption. The staff-related expenses are vital to ensure that your employees can transition to the new system comfortably and that their productivity remains intact during the transition.
As a healthcare facility, the success of your Electronic Health Record adoption solely depends on how prepared your staff is, whether you are running a small practice or have a large facility.
A) Labor Cost
The setup and integration will require considerable involvement of your internal team, from system testing and data migration to administrative preparation, plenty of behind-the-scenes work involving dedicated man-hours.
- Wages and salaries for staff involved in implementation tasks
- Project managers or coordinators hired specifically for deployment
- Time investment from physicians and clinical leaders
These labor costs can add up quickly, particularly in larger practices that affect many departments.
B) EHR Training & Onboarding Expenses
One of the most significant investments when deploying an EHR is training. Well-trained employees also help minimize errors, which leads to faster adoption and better outcomes in the long run.
Typical EHR training costs include:
- Vendor-led sessions (virtual or in-person)
- Training materials and handbooks
- Access to webinars, simulations, or video tutorials
- Support for ongoing education and role-specific learning
Depending on the complexity of your EHR system, you may also need refresher courses or additional training for updates and new features.
C) Opportunity Costs
Transitioning to a new system is time-consuming, and during this time, your team may be working below its full potential. This is where opportunity costs kick in.
- Clinicians may see fewer patients while they learn the software.
- Administrative teams may take longer to process claims or manage scheduling.
- Productivity may dip in the short term, impacting revenue.
By knowing and planning for these hidden productivity costs, you can keep your business steady while your team adjusts.
Why Staff-Related Costs Matter?
EHR systems don’t function without operational support. Your platform runs on its people, and you should know that investing in their training and support isn’t a cost; it’s an investment in long-term ROI. Focusing on ensuring staff are ready can significantly reduce frustration, increase system adoption rates, and improve patient care.
Pro Tip: Find an EHR vendor who provides a package that includes training and support to help your practice make the transition smoothly.
4. Unexpected Costs
Many EHRs have predictable costs, but others can surprise you on the deployment journey. If you are not prepared for the expenses incurred in the due process, it can significantly impact your timeline, budget, and overall success.
Understanding what hidden costs to watch out for will ensure you avoid surprises and keep within the scope during your EHR transition.
A) Change Management Expenses
Implementing a new EHR system is more than a technology upgrade; it’s a cultural shift. If you don’t invest in proper change management, the project can be stalled for weeks with staff resistance, workflow confusion, and low user adoption.
Typical costs here may include:
- Hiring consultants to lead change management strategies
- Creating internal communications and engagement materials
- Hosting team meetings or workshops to manage expectations
- Developing policies for new digital workflows
By proactively budgeting for change management support, you can help ensure a smoother, more successful adoption of your EHR.
B) Compliance & Regulatory Costs
EHR systems need to meet general industry regulations such as HIPAA, HL7, GDPR, and any other security standards relevant to your area and type of practice.
Your compliance-related expenses may include:
- Investing in data encryption and backup systems
- Hiring experts for regulatory audits or risk assessments
- Adapting your EHR settings to meet industry certification requirements
- Keeping up with changing healthcare data laws.
Ignoring compliance during EHR rollout can lead to fines, audits, or data breaches—all of which are far more costly than proactive preparation.
C) Integration & Interoperability Costs
For EHRs to be as beneficial to your practice as possible, they must integrate smoothly with your current tech stack (billing software, lab systems, telehealth platforms, scheduling tools, etc.).
These integration-related costs can include:
- Developer fees to customize EHR connections
- APIs or plug-ins to enable data sharing and real-time sync
- Extra configuration for third-party software compatibility
If your vendor doesn’t offer built-in interoperability, be prepared to pay more for tech support and healthcare development platform.
Also Read: Healthcare App Development Cost
Benefits Of EHR Implementation
EHRs offer real, measurable value to healthcare practices far beyond compliance and digital convenience. When done right, they optimize workflows, reduce costs, and enhance the patient experience.
Health Affairs reports that practices can often recoup the cost of implementing an EHR in 2.5 years. Then, over time, they earn an average of $23,000 in net benefits per full-time employee each year, demonstrating that EHRs can deliver ongoing ROI in the long term.
Let’s explore some of the most powerful benefits:
1. Reduced Paperwork
With an EHR system implemented, your team won’t have to search for paper charts or fill out forms by hand anymore. All critical patient information is available with a few clicks — a time-saver that significantly reduces human error. Billing, charting, and documentation tasks become streamlined and precise, allowing your employees to concentrate on treating patients instead of paperwork.
2. Smarter Practice Management
Electronic Health Record (EHR) systems integrate essential clinical and administrative functions—including appointment scheduling, progress note entry, billing, and medical coding—within a single digital interface. It dramatically cuts the manual work, minimizes errors, and provides an efficient running of daily operations in all departments.
For instance, if a patient’s visit is logged in real time, the same system can simultaneously log their medical history, produce billing codes, and schedule follow-up appointments. All of this can happen without separate software tools or another round of data entry. Such deep automation not only increases staff productivity but also improves the patient experience overall due to faster service and better coordination of care.
Practices that embrace centralized EHR workflows typically report faster turnaround times, more accurate documentation, and improved compliance with healthcare regulations.
3. Empowered Communication and Real-Time Communication
Electronic Health Records (EHRs) are centralized, secure systems for the storage of patient data, whether cloud-based or on-premise, which make real-time access and seamless sharing of information possible across care teams. Be it lab results, imaging reports, referrals, or medication updates, the data is immediately available to authorized providers.
This level of accessibility significantly improves care coordination, especially in multidisciplinary practices or emergency scenarios. For instance, if a primary care physician refers a patient to a specialist, the specialist can review the patient’s full medical history, test results, and notes before the appointment, even before the patient arrives. This eliminates the need for repeated diagnostics and allows clinicians to make faster, more informed decisions.
4. Enhanced Data Accessibility
Data accessibility for both providers and patients has arguably been one of the most prominent forces driving the widespread adoption of Electronic Health Records (EHRs). Electronic health record systems provide secure, real-time access for providers to medical records from any approved device, greatly enhancing the quality and continuity of care.
For healthcare providers, this translates to accessing vital patient information — including medical history, lab results, and prescriptions — from anywhere with an internet connection. This removes barriers due to physical records or systems being siloed, which can be especially helpful for physicians who work across multiple sites or provide telehealth services.
For patients, EHR systems give them the ability to access their health data digitally, Individuals can access their test results, treatment plans, vaccination status, and other information through secure patient portals. This not only improves transparency but also allows patients to participate in their health care choices.
Top EHR Systems
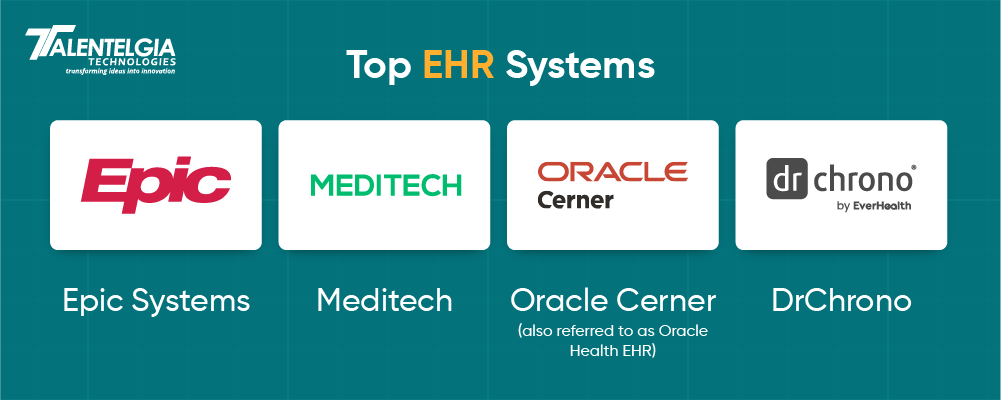
1. Epic Systems
Epic Systems is known as a pioneer in EHR and is trusted by some of the largest hospitals, health networks, and academic medical centers in the world. Founded in 1979, Epic has established a reputation for enabling scalable, integrated, and safe EHR solutions for every piece of the care journey.
Epic is a cloud-based EHR platform that helps care providers manage patient data digitally while staying compliant with HIPAA and other healthcare regulations. It is built for interoperability and efficiency, allowing for seamless integrations with lab systems, pharmacies, and billing tools. Epic shines in multi-specialty practices and settings with high-volume care. This is due to its focus on patient engagement, care coordination, and clinical documentation.
Epic stands as a strong, top-notch solution for healthcare organizations. It seeks long-term scalability and improved patient outcomes with its extensive customization capabilities, built-in telehealth functionality, and advanced analytics.
Why Choose Epic Systems EHR?
- Proven Track Record: Used by leading healthcare providers worldwide with decades of reliability.
- Cloud-Based & HIPAA-Compliant: Ensures secure data storage and remote access for clinicians and patients.
- Highly Scalable: Suitable for both mid-sized practices and complex, multi-site health systems.
- Strong Patient Engagement Tools: Features like MyChart keep patients connected and informed.
- Interoperable with Third-Party Systems: It easily integrates with lab, imaging, and billing software.
Top Features of Epic EHR
- MyChart Patient Portal – Gives patients 24/7 access to their health records, appointment scheduling, and direct messaging with providers.
- Built-In Telehealth – Enables virtual visits and remote care directly within the EHR interface.
- Smart Clinical Documentation – Includes voice recognition, smart phrases, and customizable templates to speed up charting.
- Population Health Management – Tools for monitoring patient outcomes and managing chronic conditions.
Cons of Epic EHR
- High Initial Investment – The cost of implementation, including licensing, IT setup, and training, can be steep for smaller practices.
- Learning Curve – Its extensive features require intensive user training and longer onboarding time.
- Complex Customization – Adapting the platform for unique workflows can demand technical expertise and time.
- IT Infrastructure Demands – Organizations must ensure they have robust hardware and connectivity to support Epic’s performance needs.
Proven Results From Healthcare Providers Using Epic EHR
Mackenzie Health in Ontario, Canada, is transforming the patient registration experience by seamlessly incorporating Epic’s MyChart and self-service kiosks into its check-in process. This has resulted in quicker, more intuitive, and patient-centered workflows.
- 13 Minutes Saved per Patient
Patients at Mackenzie Health spend 80% less time at registration and save an average of 13 minutes during our visits.
- 90 %+ Kiosk Adoption
For scheduled visits, more than 90% of patients check-in notes into the self-service kiosks, enabling a smooth, efficient, and standardized check-in.
- No Staffing Changes For High-Volume Efficiency
An efficient, hybrid registration model allows the hospital to service a rising number of patients without increasing the front desk headcount.
Mackenzie Health’s success with digital transformation and Epic EHR earned them an HIMSS Stage 7 certification—a testament to their leadership in leveraging health IT for better care and experience.
2. Meditech
Meditech is one of the longest-tenured health IT providers, providing fully integrated electronic health record (EHR) solutions designed for small to medium hospitals and health systems. Founded in 1969, Meditech has a legacy of innovation, adapting and changing over the years to meet the ever-evolving needs of the clinician, administrator, and patient.
The Meditech EHR platform is built to support simplified day-to-day workflows, better clinical decision-making, and evolving the patient-provider partnership. Its on-premise and cloud-enabled systems are used for many core functions. This includes clinical documentation, scheduling, charting, revenue cycle management, and patient engagement.
Why Choose Meditech EHR?
- Legacy & Trust: Over 50 years of experience serving hospitals nationwide.
- Interoperable & Integrated: Connects seamlessly with external health systems for coordinated care.
- Cloud & On-Premise Options: Flexible deployment based on your infrastructure needs.
- MaaS (MEDITECH as a Service): Subscription-based EHR ideal for smaller hospitals.
Top Features of Meditech EHR
- Comprehensive Patient Portal – Enables patients to manage appointments, access records, and communicate with care teams.
- Revenue Cycle Management – Streamlines billing, claims, and reimbursements to enhance financial performance.
- Robust Analytics Tools – Deliver actionable insights through performance dashboards and clinical reporting.
- Regulatory Compliance – Built-in compliance with HIPAA and other industry standards ensures safe and secure patient data handling.
Proven Results From Healthcare Providers Using Meditech
30% Reduction in Hospital-Acquired Infections
Southern Ohio Medical Center used Meditech’s predictive analytics and clinical surveillance tools to reduce rates of hospital-acquired C. difficile infections by 30%. This led to enhanced patient safety and a decrease in inpatient complications.
35% Increase in Patient Engagement & Reduced No-Show Rates
Hancock Health employed Meditech’s patient engagement platform to optimize appointment management and communications. This resulted in a significant 35% rise in patient engagement and a sharp decrease in no-show rates.
Clinicians save 30% time on clinical tasks
Thanks to Meditech’s optimized clinical workflows & intuitive interface, Major Health Partners saw a 30% time savings in home medication verification within the emergency department.
Diabetic Ketoacidosis Resolution 25% Faster
Appalachian Regional Healthcare utilized Meditech’s decision-support and care coordination technology to improve care outcomes by decreasing the time it takes to resolve cases of diabetic ketoacidosis (DKA) by 25%.
3. Oracle Cerner
Oracle Cerner, which is now Oracle Health EHR, originated as Cerner over four decades ago. The 2022 acquisition by Oracle allowed the company to rebrand the platform and introduce a slew of new technology and innovation. Oracle Health EHR is a cloud-based, scalable, fully integrated electronic health record (EHR) solution for 55 specialties.
It is also a future-focused platform that enables healthcare providers of all sizes—from small clinics to large hospital systems—to improve clinical efficiency, care coordination, and digital transformation.
Why Choose Oracle Health EHR?
- Scalable Infrastructure: Tailored solutions for small practices, community hospitals, and large enterprise systems.
- Powerful Cloud-Based Tools: Fully integrated with Oracle Cloud for enhanced scalability and performance.
- Future-Ready Analytics: AI, machine learning, and population health tools for proactive care.
- Secure & Compliant: HIPAA-compliant with advanced data security measures.
Top Features Of Oracle Health EHR
- Population Health Management: Risk stratification, predictive analytics, and proactive intervention planning.
- Revenue Cycle Management: Streamlined billing and reimbursement tools to boost financial outcomes.
- Telehealth Integration: Built-in support for remote care delivery and patient monitoring.
- Patient Portal (MyCerner): Gives patients real-time access to health data, messaging, and scheduling.
Client Success Story: EHS Reduces Antibiotic Use and Saves AED 13M Using Oracle EHR
Emirates Health Services (EHS) revamped its antibiotic stewardship with support from Oracle Health EHR. Clinical protocols were built directly into the Wareed EHR system, allowing greater control over empirical antibiotic prescribing based on the best available evidence.
Before this EHR-based intervention, the average duration of empirical antibiotics given was 4.4 days. Physicians received real-time reminders to reassess antibiotic use with the new protocol-embedded antibiotic review alerts set at the 72-hour mark. This greatly decreased unnecessary prescriptions and enhanced patient safety.
Results:
- Empirical antibiotic consumption dropped by over 5X
- Average prescription duration fell to 2.8 days
- EHS saved AED 13,171,322 in antibiotic-related costs within a year.
Jini Stephen, Health Information Systems Specialist at EHS, emphasized the importance of this initiative:
“Through the Oracle Health antibiotic stewardship program, we safeguard our present by preserving the effectiveness of antibiotics, helping to ensure a healthier future for our generations.”
4. Dr Chorno
DrChrono is a cloud-based Electronic Health Record (EHR) solution designed for small to mid-sized medical practices. DrChrono (2009) — EHR, practice management, medical billing, and telehealth in one platform accessible from iPad, iPhone, or Desktop. It’s the first EHR to create a native app for iPad and is a leader in the mobile-first movement in healthcare technology.
Designed for flexibility and ease of use, DrChrono allows providers to deliver patient care and remains compliant with industry standards like HIPAA and MACRA. The platform is used in more than 40 medical specialties, from billing to administrative functions to clinical workflows, forms, and charting tools, allowing for extensive customization.
Why Choose DrChrono EHR?
- Mobile-First Flexibility: Optimized for iPad and iPhone—ideal for providers on the go.
- Highly Customizable: Tailor forms, charting templates, and workflows to fit your practice.
- Integrated Telehealth: Seamlessly conduct virtual visits directly through the platform.
- All-in-One Billing: End-to-end revenue cycle management included with EHR.
Top Features of DrChrono
- Custom Clinical Forms: Build or modify templates to match your specialty or workflow needs.
- Real-Time Eligibility Checks: Instantly verify patient insurance before the appointment.
- Patient Portal: Secure access for patients to book appointments, view test results, and message providers.
- eRx and EPCS: Electronic prescribing, including controlled substances.
Case Study: How a Boston Family Practice Boosted Revenue with DrChrono’s Managed Billing Services
A Boston-based family practice dramatically improved its revenue performance by switching from an in-house biller to DrChrono’s Managed Billing Services—all without increasing patient volume or appointments.
This transformation wasn’t about working more; it was about collecting smarter.
Previously, the clinic relied on an in-house billing team. While their monthly insurance-eligible billing totaled $26,000, they were only collecting $18,200, with a steep billing overhead of $6,176/month. After accounting for staff costs and inefficiencies, the net annual collections totaled just $144,288.
Upon switching to DrChrono’s end-to-end managed billing solution, the same $26,000 in billables now yielded $22,100/month in collections—a 21% increase in recovered revenue. Even better, the billing cost dropped dramatically to just $1,820/month.
With optimized claims management, reduced denials, and faster reimbursements, the practice saw its net annual collections jump to $243,360—a 68% increase in take-home revenue.
Conclusion
EHR implementation is more than a financial investment—it’s a strategic leap toward smarter, data-driven healthcare. While the upfront and hidden costs can be significant, the long-term value lies in enhanced patient outcomes, streamlined workflows, and greater compliance confidence. To make the most of your investment, choose a system that scales with your needs, ensure your team is fully supported during the transition, and don’t underestimate the power of post-implementation optimization. When done right, your EHR can become the silent engine behind exceptional care.


 Healthcare App Development Services
Healthcare App Development Services
 Real Estate Web Development Services
Real Estate Web Development Services
 E-Commerce App Development Services
E-Commerce App Development Services E-Commerce Web Development Services
E-Commerce Web Development Services Blockchain E-commerce Development Company
Blockchain E-commerce Development Company
 Fintech App Development Services
Fintech App Development Services Fintech Web Development
Fintech Web Development Blockchain Fintech Development Company
Blockchain Fintech Development Company
 E-Learning App Development Services
E-Learning App Development Services
 Restaurant App Development Company
Restaurant App Development Company
 Mobile Game Development Company
Mobile Game Development Company
 Travel App Development Company
Travel App Development Company
 Automotive Web Design
Automotive Web Design
 AI Traffic Management System
AI Traffic Management System
 AI Inventory Management Software
AI Inventory Management Software
 AI Software Development
AI Software Development  AI Development Company
AI Development Company  AI App Development Services
AI App Development Services  ChatGPT integration services
ChatGPT integration services  AI Integration Services
AI Integration Services  Generative AI Development Services
Generative AI Development Services  Natural Language Processing Company
Natural Language Processing Company Machine Learning Development
Machine Learning Development  Machine learning consulting services
Machine learning consulting services  Blockchain Development
Blockchain Development  Blockchain Software Development
Blockchain Software Development  Smart Contract Development Company
Smart Contract Development Company  NFT Marketplace Development Services
NFT Marketplace Development Services  Asset Tokenization Company
Asset Tokenization Company DeFi Wallet Development Company
DeFi Wallet Development Company Mobile App Development
Mobile App Development  IOS App Development
IOS App Development  Android App Development
Android App Development  Cross-Platform App Development
Cross-Platform App Development  Augmented Reality (AR) App Development
Augmented Reality (AR) App Development  Virtual Reality (VR) App Development
Virtual Reality (VR) App Development  Web App Development
Web App Development  SaaS App Development
SaaS App Development Flutter
Flutter  React Native
React Native  Swift (IOS)
Swift (IOS)  Kotlin (Android)
Kotlin (Android)  Mean Stack Development
Mean Stack Development  AngularJS Development
AngularJS Development  MongoDB Development
MongoDB Development  Nodejs Development
Nodejs Development  Database Development
Database Development Ruby on Rails Development
Ruby on Rails Development Expressjs Development
Expressjs Development  Full Stack Development
Full Stack Development  Web Development Services
Web Development Services  Laravel Development
Laravel Development  LAMP Development
LAMP Development  Custom PHP Development
Custom PHP Development  .Net Development
.Net Development  User Experience Design Services
User Experience Design Services  User Interface Design Services
User Interface Design Services  Automated Testing
Automated Testing  Manual Testing
Manual Testing  Digital Marketing Services
Digital Marketing Services 
 Ride-Sharing And Taxi Services
Ride-Sharing And Taxi Services Food Delivery Services
Food Delivery Services Grocery Delivery Services
Grocery Delivery Services Transportation And Logistics
Transportation And Logistics Car Wash App
Car Wash App Home Services App
Home Services App ERP Development Services
ERP Development Services CMS Development Services
CMS Development Services LMS Development
LMS Development CRM Development
CRM Development DevOps Development Services
DevOps Development Services AI Business Solutions
AI Business Solutions AI Cloud Solutions
AI Cloud Solutions AI Chatbot Development
AI Chatbot Development API Development
API Development Blockchain Product Development
Blockchain Product Development Cryptocurrency Wallet Development
Cryptocurrency Wallet Development About Talentelgia
About Talentelgia  Our Team
Our Team  Our Culture
Our Culture 
 Healthcare App Development Services
Healthcare App Development Services Real Estate Web Development Services
Real Estate Web Development Services E-Commerce App Development Services
E-Commerce App Development Services E-Commerce Web Development Services
E-Commerce Web Development Services Blockchain E-commerce
Development Company
Blockchain E-commerce
Development Company Fintech App Development Services
Fintech App Development Services Finance Web Development
Finance Web Development Blockchain Fintech
Development Company
Blockchain Fintech
Development Company E-Learning App Development Services
E-Learning App Development Services Restaurant App Development Company
Restaurant App Development Company Mobile Game Development Company
Mobile Game Development Company Travel App Development Company
Travel App Development Company Automotive Web Design
Automotive Web Design AI Traffic Management System
AI Traffic Management System AI Inventory Management Software
AI Inventory Management Software AI Software Development
AI Software Development AI Development Company
AI Development Company ChatGPT integration services
ChatGPT integration services AI Integration Services
AI Integration Services Machine Learning Development
Machine Learning Development Machine learning consulting services
Machine learning consulting services Blockchain Development
Blockchain Development Blockchain Software Development
Blockchain Software Development Smart contract development company
Smart contract development company NFT marketplace development services
NFT marketplace development services IOS App Development
IOS App Development Android App Development
Android App Development Cross-Platform App Development
Cross-Platform App Development Augmented Reality (AR) App
Development
Augmented Reality (AR) App
Development Virtual Reality (VR) App Development
Virtual Reality (VR) App Development Web App Development
Web App Development Flutter
Flutter React
Native
React
Native Swift
(IOS)
Swift
(IOS) Kotlin (Android)
Kotlin (Android) MEAN Stack Development
MEAN Stack Development AngularJS Development
AngularJS Development MongoDB Development
MongoDB Development Nodejs Development
Nodejs Development Database development services
Database development services Ruby on Rails Development services
Ruby on Rails Development services Expressjs Development
Expressjs Development Full Stack Development
Full Stack Development Web Development Services
Web Development Services Laravel Development
Laravel Development LAMP
Development
LAMP
Development Custom PHP Development
Custom PHP Development User Experience Design Services
User Experience Design Services User Interface Design Services
User Interface Design Services Automated Testing
Automated Testing Manual
Testing
Manual
Testing About Talentelgia
About Talentelgia Our Team
Our Team Our Culture
Our Culture















 Write us on:
Write us on:  Business queries:
Business queries:  HR:
HR: 




